What you’ll learn:
- Ozempic® is FDA-approved for type 2 diabetes, but it’s also commonly prescribed off-label to support weight loss.
- Its active ingredient, semaglutide, mimics a natural hormone that helps regulate blood sugar, reduce appetite, and slow digestion, called GLP-1.
- While people can lose weight with Ozempic, Wegovy, its sister medication, contains the same active ingredient, can be prescribed at a higher dose, and is FDA-approved for weight loss.
Ozempic® has become more than just a prescription—it’s practically a household name. You’ve probably seen it mentioned in celebrity interviews, trending across social media, or popping up in conversations about modern weight loss. Behind the buzz, Ozempic® is actually a medication originally designed to help manage type 2 diabetes, not weight loss.
It belongs to a class of drugs known as GLP-1 receptor agonists, which mimic a hormone your body produces called glucagon-like peptide (GLP-1 for short). When you eat, GLP-1 helps regulate blood sugar, appetite, and digestion. While Ozempic was first used for diabetes, many people taking it noticed a side effect that changed everything: significant weight loss.
That discovery helped reshape how we think about long-term weight management. It also led to the creation of Wegovy®, Ozempic’s sister medication, which uses the same active ingredient (semaglutide) but is FDA-approved specifically for weight management.
So what’s the real difference between the two? And how does Ozempic® actually work? We’ll cover how it helps with weight loss, how much you can expect to lose, what it costs, and how it stacks up next to Wegovy® and other GLP-1 medications.
What is Ozempic® and how does it work?
The active ingredient in Ozempic® is semaglutide. It enters the body through a once-weekly shot and mimics the hormone GLP-1 to help lower appetite, slow digestion, and stabilize blood sugar.
What is GLP-1 and what does it do?
Your body already makes GLP-1 on its own. Balanced meals with protein and healthy fats, and exercise can increase GLP-1 levels naturally. It’s released by special cells in your intestines, called L-cells, after you eat. These cells respond to nutrients and send signals that help manage digestion and appetite.
There are GLP-1 receptors in several areas of the body that influence weight and blood sugar.
- In the pancreas, they help your body release more insulin when blood sugar levels rise and lower another hormone called glucagon.
- In the brain, especially in areas that control hunger and fullness like the hypothalamus, they help you feel satisfied sooner and reduce appetite.
- In the digestive system, they help slow the rate food leaves your stomach, which keeps you feeling fuller for longer.
The semaglutide in Ozempic® (and Wegovy®) mimics GLP-1 to reduce appetite, slow digestion, and stabilize blood sugar, helping people lose weight or manage diabetes.
Learn more about how semaglutide works for weight loss.
Why did Ozempic® become popular for off-label weight loss?
The FDA first approved Ozempic® in 2017 for type 2 diabetes, and people taking it quickly noticed it often led to significant weight loss. By 2020, studies and online chatter about its slimming effects were already growing. When Wegovy® was approved for weight management in 2021, media coverage helped grow semaglutide as a significant advancement in weight loss.
How much weight can I lose taking Ozempic®?
People taking Ozempic® off-label tend to see steady progress over several months.
In a large clinical trial, people on the highest dose of Ozempic® (2 mg weekly) lost an average of about 15 pounds, roughly 7% of their body weight, over 40 weeks. Those on the 1 mg dose lost around 13 pounds, or about 6% of their body weight, during the same period.
The study looked at adults with type 2 diabetes who were already taking metformin. The main goal was to see how well the medication improved blood sugar levels, while weight loss was tracked as a secondary benefit.
How much weight can I lose with Wegovy?
A higher dose of semaglutide is available with Wegovy®. It can be prescribed up to 2.4 mg and has shown average reductions of around 15% of starting body weight in clinical trials. The study focused specifically on weight management and combined semaglutide treatment with behavioral support.
Remember, these are averages; some people will lose less, and some will lose more. People lose the most weight when they focus on eating a balanced, lower-calorie diet and moving more. It’s also important what they eat. Choosing nutrient-dense foods helps support steady, sustainable weight loss (1 to 2 pounds per week) while keeping energy up and maintaining muscle.
Learn more about what to eat while taking Ozempic.
How quickly will I lose weight with semaglutide?
You might start to see small changes by week 4, during the introductory 0.25 mg dose. This phase is mostly about letting your body adjust, so early weight loss is usually minimal.
Studies have also shown that weight loss with semaglutide is dose-dependent, meaning progress tends to build as your dosage increases. Here’s what the average progress looked like for people taking different semaglutide doses over time, according to a weight loss study:
| Dose group | Weight loss in 3 months | Weight loss in 6 months |
|---|---|---|
| Lower dose (0.25, 0.5, and 1 mg) | 5% | 9% |
| Higher dose (1.7 and 2.4 mg) | 7% | 12% |
Ozempic®: Cost and insurance considerations
Ozempic® can be life-changing for many people, but it’s also a significant financial commitment. What you’ll pay for the medication can vary depending on where you fill your prescription and what kind of insurance you have, so it’s worth looking into your coverage before starting treatment.
The list price for Ozempic® is around $998 per month, regardless of the dose (0.25 mg, 0.5 mg, 1 mg, or 2 mg). Your actual cost depends on your insurance plan, eligibility for discounts, and where you fill your prescription.
Does insurance ever cover Ozempic®?
Insurance coverage for Ozempic® largely depends on why it’s prescribed and the type of plan you have. Some private or employer-sponsored plans are more likely to cover Ozempic® when it’s prescribed for type 2 diabetes, but it will rarely, if ever, be covered for off-label weight loss use. Weight loss medication isn’t commonly covered by insurance.
When prescribed for diabetes, Medicare and Medicaid coverage varies by state and plan, and out-of-pocket costs can change depending on your deductible. To avoid surprises, it’s best to check directly with your insurance provider to see how Ozempic® is listed on your plan’s preferred drug list.
Can you save on Ozempic® with manufacturer discounts?
There are savings options that can help lower your monthly payment for Ozempic®.
- If you have insurance: Those with commercial or employer-based insurance may qualify for the Ozempic® Savings Card, which can reduce your cost to as little as $25 for up to a 3-month supply (for up to 48 months). This offer isn’t available for Medicare or Medicaid, but it can make a big difference for privately insured users. Again, this is when it’s prescribed for diabetes.
- If you don’t have insurance coverage: You can get Ozempic® through the NovoCare® pharmacy for $499 per month.
These programs can change, so it’s always a good idea to confirm your eligibility through Novo Nordisk’s official website or your pharmacy before filling your prescription.
Learn more about the cost of Ozempic®.
Is there a generic for Ozempic®?
No, there’s currently no generic version of Ozempic® available. The medication is still under patent protection by its manufacturer, Novo Nordisk, which means other companies can’t legally produce a generic equivalent yet.
In the U.S., the main patent on semaglutide is set to expire around 2032. In Canada, however, the timeline is shorter, with protection expected to end by January 2026 following a missed maintenance fee.
Once these patents expire, generic options may enter the market, potentially lowering the cost and increasing access for more people.
Rx weight loss, the right way, with Noom
Get access to prescription weight loss medication with Noom.Who can prescribe Ozempic®?
Ozempic® is a prescription-only medication, so it must be prescribed by a licensed healthcare provider. In most cases, that includes primary care physicians, endocrinologists, nurse practitioners, and physician assistants.
Because Ozempic® is approved to treat type 2 diabetes, it’s typically prescribed to people with that condition. But some healthcare providers prescribe it off-label for weight management, particularly if you have a BMI of 30 or higher, or 27 or higher with high blood pressure or high cholesterol.
If you’re interested in trying Ozempic® or a similar GLP-1 medication, your provider will likely review your medical history, blood work, and current medications to make sure it’s a safe fit. They can also help determine if another semaglutide-based option—like Wegovy®—is more appropriate for you.
Learn more about how Ozempic is prescribed.
Ozempic®: Dosage and how to take it
Ozempic® is taken once a week using a prefilled injection pen. You inject it just under the skin, typically in your abdomen, thigh, or upper arm. The process may sound intimidating at first, but most people find it quick and easy once they get used to it. The needle is tiny, and the injection usually causes little to no discomfort.
Everyone starts with the lowest dose. The dose will gradually increase to help your body adjust and reduce the likelihood of side effects like nausea, vomiting, or stomach pain.
Here’s a general overview of how dosing typically works. Your provider may keep you at a lower dose longer if you are losing steady weight or have issues with side effects:
| Week | Dose (weekly) | What to expect |
|---|---|---|
| Weeks 1-4 | 0.25 mg | Introductory stage to help your body adjust to semaglutide and minimize side effects. |
| Weeks 5-8 | 0.5 mg | Dose increases as your body adapts; some people begin noticing early weight changes. |
| Week 8+ (as needed) | 1 mg | Your provider may raise your dose further depending on your progress and tolerance. |
| Highest dose | 2 mg once weekly | Maximum approved Ozempic® dose for continued treatment. |
If you need a higher semaglutide dose to continue losing weight, your provider may switch you to Wegovy®, which is approved for weight management at doses up to 2.4 mg.
Learn more about Ozempic® dosage & Wegovy® dosage.
Ozempic®: Side effects and safety
Since Ozempic® works through your gut hormones, some digestive symptoms, like nausea or constipation, are expected when you first start the medication or when your dose is changed. We’ll break down which side effects are most common, which ones are worth a quick check-in with your doctor, and which require immediate attention.
The most common side effects of Ozempic®
Most people experience mild side effects as their body adjusts to the initial dose or when their dose is increased. These side effects typically fade with time as your system gets used to the medication.
The most common side effects are:
- Nausea
- Vomiting or diarrhea
- Abdominal pain
- Constipation
If something feels off or doesn’t seem to be improving, check in with your healthcare provider for guidance.
Get more information on staying safe while taking Ozempic.
Rare but serious side effects
Serious side effects from Ozempic® are uncommon, but it’s important to recognize them early and act fast if they occur:
- Pancreatitis – Symptoms include intense abdominal pain that radiates to the back, often accompanied by nausea or vomiting. If you notice these symptoms, stop using Ozempic® and contact your healthcare provider right away. Learn more about the connection between Ozempic® and pancreatitis.
- Gallbladder issues – People experiencing pain in the upper right belly, fever, or yellowing of the skin or eyes can point to gallstones or gallbladder inflammation. Seek emergency care right away if these symptoms appear.
- Kidney issues – Dehydration from vomiting or diarrhea may strain your kidneys. Watch for swelling, fatigue, or less frequent urination, and get emergency medical attention if these happen.
- Severe stomach symptoms – Persistent nausea, bloating, or abdominal pain that won’t go away should be checked out right away.
- Severe allergic reaction – Get emergency help for facial or throat swelling, rash, trouble breathing, or a fast heartbeat.
- Low blood sugar (hypoglycemia) – Hypoglycemia is more likely if you’re also taking insulin or sulfonylureas. Signs include shakiness, sweating, or confusion. Get immediate medical attention. Learn more about the connection between Ozempic® and hypoglycemia.
- Thyroid cancer or tumors – Tell your healthcare provider right away if you notice a lump or swelling in your neck, hoarseness, difficulty swallowing, or shortness of breath, as these can be warning signs of a thyroid tumor. Learn more about how Ozempic® is linked to thyroid health.
If you notice any of these warning signs or any new or concerning symptoms, stop using Ozempic® and contact your healthcare provider immediately.
Learn more about Ozempic® side effects and get the complete safety info for Ozempic.
Who shouldn’t take Ozempic®?
Ozempic® isn’t right for everyone. Your healthcare provider will review your health history carefully before prescribing it.
You shouldn’t take Ozempic® if:
- You or someone in your family has been diagnosed with medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia type 2 (MEN 2).
- You have a known allergy to semaglutide or any of the ingredients in Ozempic®.
- Are pregnant, planning a pregnancy, or breastfeeding.
Your doctor will decide if Ozempic® is right for you if you:
- Have a history of pancreatitis.
- Live with severe digestive issues such as gastroparesis.
Overdose risks and symptoms
Taking more than your prescribed dose of Ozempic® can lead to serious side effects. Possible signs of an overdose can include severe nausea, persistent vomiting, dizziness, or symptoms of low blood sugar, like shakiness, sweating, confusion, or a rapid heartbeat.
If you think you’ve taken too much, contact your healthcare provider, Poison Control (1-800-222-1222), or go to the nearest emergency room right away. Overdoses are uncommon but can be dangerous, so always follow your prescribed dosing schedule and check with your provider before making any changes.
Ozempic®: Tips for best weight loss results
Taking Ozempic® the right way can help you get the most out of your treatment, both in how much weight you lose and how comfortable you feel throughout the process. Here are some tips to keep in mind:
| Issue | Tips |
|---|---|
| Timing your dose | Inject Ozempic® once a week, on the same day each week. It can be taken with or without food, so you can choose the time of day that fits best with your routine.Try pairing your dose with a recurring weekly task to make it easier to remember. |
| If you miss a dose | Take it as soon as you remember, as long as it’s within 5 days of your usual injection day. If it’s been more than 5 days, skip that dose and take your next one on your regular schedule. Don’t double up to “catch up.” |
| Injection placement | Inject under the skin of your abdomen, thigh, or upper arm, whichever feels most comfortable. Rotate injection sites each week to prevent irritation. If you prefer one area, like your stomach, avoid using the same spot every time. |
| How to inject | Always check that the liquid in your pen is clear and particle-free before use. Wash your hands, clean the area with an alcohol swab, and attach a new needle for every injection. Hold the pen at a 90-degree angle, press the button, and keep it in place for about 6 seconds to make sure you get the full dose. |
| Managing side effects | Mild nausea is common when you first start the medication or when your dose increases. Try injecting at night so you can sleep through discomfort, eat smaller meals, and stay hydrated. |
| Supporting your results | Ozempic® works best alongside healthy habits. Focus on balanced meals, regular movement, and consistent sleep. Keeping track of your progress and recognizing small achievements can keep you motivated along the way. |
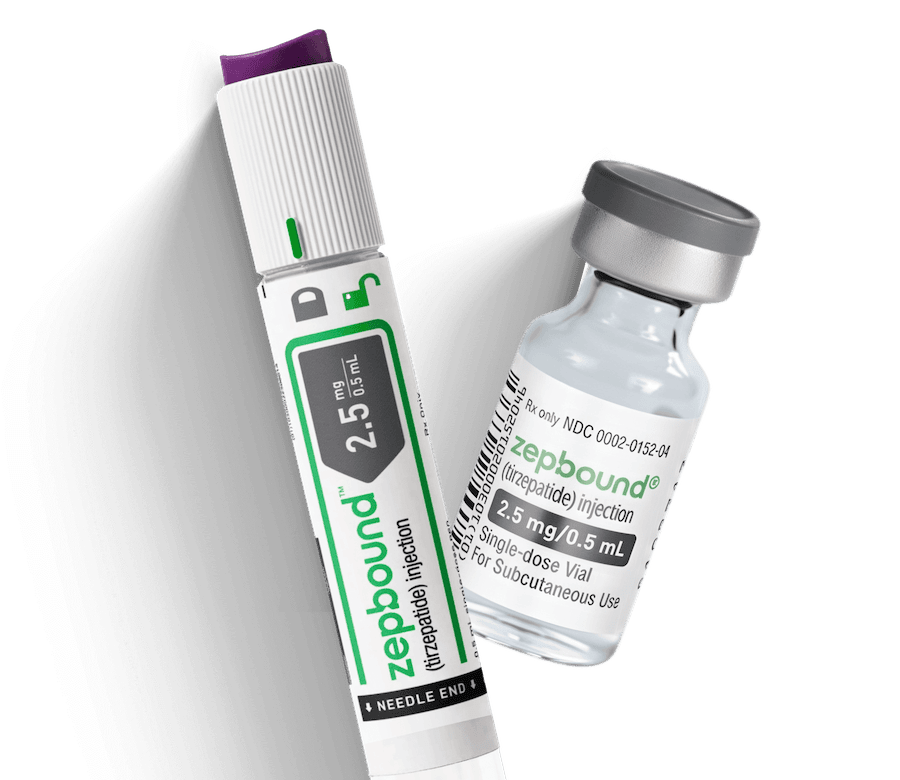
Ozempic® vs. other GLP-1s: Weight loss potential
Studies show a range of results across GLP-1 medications used for weight management. Here’s where Ozempic® fits among the most commonly prescribed options:
| Medication | Study length | Average weight loss |
|---|---|---|
| Semaglutide – 2 mg (Ozempic®) (off-label) | 40 weeks | 7% |
| Semaglutide – 2.4 mg (Wegovy®) | 68 weeks | 15% |
| Tirzepatide – 15 mg (Zepbound®) | 72 weeks | 21% |
| Liraglutide – 3 mg (Saxenda®) | 56 weeks | 6% |
| Dulaglutide – 4.5 mg (Trulicity®) (off-label) | 36 weeks | 5% |
While Ozempic® is effective and widely used, when it’s used for weight loss, that’s an off-label use. Newer or higher-dose GLP-1 medications like Wegovy® and Zepbound® are specifically approved for weight management.
Your healthcare provider can help determine whether continuing Ozempic® off-label or switching to another weight loss option best fits your goals and overall health plan.
Want to know more about how Ozempic® stacks up to these other medications? Check out:
- Ozempic® vs. Zepbound®
- Ozempic® vs. Mounjaro®
- Ozempic® vs. Trulicity®
- Rybelsus® vs. Ozempic®
- Saxenda® vs. Ozempic®
- Ozempic® vs. Victoza®
Frequently asked questions about Ozempic®
If you’re thinking about using Ozempic® for weight loss, you’re likely wondering all sorts of things about the medication. These FAQs cover the top questions people ask about Ozempic®, helping you understand what to expect when you start taking it.
Can you drink alcohol while taking Ozempic®?
You can have alcohol in moderation while using Ozempic®, but it’s best to be careful. Drinking can make side effects like nausea or dizziness feel stronger, and it may also cause your blood sugar to drop, especially for those managing diabetes or taking other glucose-lowering medications.
Learn more about drinking alcohol and taking Ozempic®.
How long can you safely take Ozempic®?
Ozempic® is meant to be taken long-term. The longest studies so far have tracked people for about two years, showing that it can safely support weight loss and blood sugar control over time. Your doctor will help decide how long it makes sense for you to stay on it.
Learn more about how long you can safely stay on Ozempic® for weight loss.
Can you stop taking Ozempic® at any time?
It’s not recommended to stop Ozempic® suddenly without talking to your doctor. Since appetite and hunger signals tend to return to normal once you stop, it’s possible to regain weight. If you and your provider decide it’s time to come off the medication, tapering your dose slowly can make the transition smoother and help your body adjust.
Learn more about how to stop taking Ozempic® safely.
What kind of diet and exercise plan works best with Ozempic®?
A balanced plan combining lean protein, healthy fats, fiber, and moderate portions works best alongside Ozempic®. Pair that with strength training or resistance work and regular movement; studies suggest this helps preserve muscle while you lose weight.
Learn more about what to eat on Ozempic® to support steady weight loss.
Does Ozempic® cause muscle loss, and how can you prevent it?
Ozempic® itself doesn’t cause muscle loss, but it can happen as part of weight loss in general. You can help maintain muscle by eating enough protein, doing regular strength training, and getting good sleep so your body has what it needs to stay strong while the scale goes down.
Learn more about how to prevent muscle loss while taking Ozempic®.
What is “Ozempic face,” and how can I avoid it?
“Ozempic face” refers to a facial sagging or gaunt appearance that can happen with rapid weight loss from any cause, not just Ozempic®. While partly a natural result of losing fat, you can help reduce it by losing weight steadily (not too fast), staying hydrated, getting enough protein, and doing facial or overall strength exercises.
Learn more about what causes “Ozempic face”.
Does Ozempic® cause mood changes?
Mood changes aren’t a common side effect, but some users report shifts in mood, like signs of depression or increased anxiety. The FDA has reviewed these reports and found no clear link between GLP-1 medications like Ozempic® and mood changes. If you notice new or severe changes, talk with your healthcare provider.
Learn more about how Ozempic® may affect mood and emotions.
Can you safely pause and start Ozempic® again?
Restarting Ozempic® is possible, but it’s generally not recommended since the medication works best when used consistently. If you need to pause or restart, talk with your provider so they can adjust your dose and help you ease back into it safely.
Learn more about how to safely stop and restart Ozempic®.
How does Ozempic® interact with other medications and substances?
Ozempic® can slow digestion, which may slow how quickly your body absorbs other oral medications. If you’re on drugs for diabetes, blood pressure, or thyroid, your doses may need adjusting. Always inform your prescriber about all the medications and supplements you take.
Learn more about how Ozempic® may interact with other medications.
Do females experience different side effects when taking Ozempic®?
Some studies suggest that women may experience stronger side effects from GLP-1s, especially nausea, headaches, and dizziness. On the flip side, research also hints that females may see slightly greater weight loss results than males.
Also, because Ozempic® improves insulin sensitivity and supports weight loss, it may also increase fertility in women who previously struggled with irregular ovulation, particularly those with PCOS. If you’re pregnant, planning to become pregnant, or breastfeeding, talk with your healthcare provider before starting or continuing Ozempic®. The medication can remain in your system for several weeks, so experts recommend stopping it at least two months before trying to conceive.
Learn more about Ozempic® side effects in women.
What foods should you avoid while taking Ozempic®?
There are no strict “forbidden” foods, but it’s wise to be cautious with fried, greasy, or very spicy foods, as they may worsen digestive side effects. Also, watch out for high-calorie drinks or large portions that can undermine your weight-loss goals.
Learn more about which foods to avoid while taking Ozempic®.
Read more:
The bottom line: Ozempic® can be effective for off-label weight loss
While Ozempic® was originally developed for type 2 diabetes, it’s still a well-known option for off-label weight loss. Many people experience steady progress with it, especially when paired with healthy habits. However, some people might need to switch to Wegovy® if weight loss stalls on Ozempic®.
And, you won’t necessarily save any money on Ozempic® vs. Wegovy®. When it comes to pricing and insurance, neither is likely to be covered. While the list price of Wegovy is higher, both prescriptions can be filled through the manufacturer’s pharmacy for $499. Which one you choose comes down to the one your doctor thinks is right for you.
If you want to explore weight loss medications further, see if you qualify for Noom Med. If so, our licensed clinicians evaluate your unique health needs, prescribe medication when appropriate, and guide you through every step. You’ll also get access to Noom’s behavior-based coaching and tools that help you build sustainable, healthy habits for lasting results. Learn more about how and when Ozempic® is prescribed.
Note: Ozempic®, Mounjaro®, and Trulicity are not FDA-approved to treat obesity or for weight loss.
Why you can trust us
At Noom, we’re committed to providing health information that’s grounded in reliable science and expert review. Our content is created with the support of qualified professionals and based on well-established research from trusted medical and scientific organizations. Learn more about the experts behind our content on our Health Expert Team page.



















 Noom Team
Noom Team
 Shoshana Fishbein
Shoshana Fishbein


 Meaghan Cameron
Meaghan Cameron