What you’ll learn:
- Some research shows that using GLP-1 medications like Ozempic® and Wegovy® may be linked to rare cases of pancreatitis.
- Symptoms can come on suddenly and include severe abdominal pain, nausea, vomiting, or fever.
- Your doctor will carefully evaluate your individual risk factors before determining whether GLP-1 medications are safe for you.
Ozempic® and Wegovy® have been making headlines for their ability to help people manage type 2 diabetes (Ozempic®) and lose weight (Wegovy®). But they also come with side effects and some other potential risks.
These medications, which both contain semaglutide, work by changing how your digestive system functions. These actions can bring powerful benefits for blood sugar control and appetite regulation, but can also be linked to certain serious conditions. One of the most talked about is pancreatitis, an inflammation of the pancreas.
While pancreatitis is listed as a possible side effect of Ozempic® and Wegovy®, it’s actually very rare. Knowing who may be more at risk, what the symptoms look like, and how to recognize early warning signs can help you have informed, proactive conversations with your healthcare provider.
Let’s break down what you need to know about the connection between GLP-1 medications and pancreatitis—and how to protect your health while staying on track with your goals.
What is pancreatitis?
Pancreatitis is a condition in which the pancreas becomes inflamed. The pancreas is a glandular organ that sits just behind your stomach. It has two major jobs:
- Digestive role: It releases enzymes into the small intestine to help break down proteins, fats, and carbohydrates.
- Hormonal role: It produces hormones, most importantly insulin (which lowers blood sugar by moving glucose into cells) and glucagon (which raises blood sugar when it gets too low).
With pancreatitis, the digestive enzymes activate too early and start attacking the pancreas itself. This can lead to swelling, severe abdominal pain, nausea, and vomiting.
Types of pancreatitis
- Acute pancreatitis comes on suddenly and requires immediate medical attention. Complications can develop quickly, like infection of the pancreas, internal bleeding, or even multi-organ failure. These are the situations that can be life-threatening if not treated promptly.
- Chronic pancreatitis is ongoing inflammation that gradually damages the pancreas over time. Complications are usually different (like malnutrition, diabetes, or pancreatic cancer risk), but chronic cases can also become severe and trigger infections or internal bleeding, especially during flare-ups.
Treatment for pancreatitis
Treatment usually depends on how serious it is, with mild cases managed in the hospital with IV fluids, pain relief, and fasting for a period of time. More serious cases, on the other hand, may require longer hospital stays, antibiotics, procedures to remove gallstones, or even surgery if complications arise. The good news is that with timely medical care, many people recover fully from an acute episode, although ongoing monitoring is important to protect long-term health.
How Ozempic® and Wegovy® affect your body and the pancreas
To understand why pancreatitis sometimes happens when people use GLP-1 medications like Ozempic® and Wegovy®, it helps to look at how they work. GLP-1 receptor agonists mimic a natural gut hormone called glucagon-like peptide 1 (GLP-1 for short). GLP-1 is a hormone that helps you feel full, slows how quickly food leaves your stomach, and signals your pancreas to release insulin to keep blood sugar steady. These medications bind with GLP-1 receptors to boost your body’s built-in system for appetite, digestion, and glucose balance—one reason they’re so effective for weight loss and diabetes management.
Because the pancreas is part of the process, activating its GLP-1 receptors has raised questions about inflammation. While most people tolerate these medications well, there are some factors that can increase risk, like very high triglycerides or a history of pancreatic issues.
Rapid weight loss is another factor to consider. When the body breaks down fat quickly, it can increase the chance of developing gallstones. The gallbladder and pancreas share small ducts that carry bile and digestive enzymes into the small intestine. If a gallstone blocks one of these ducts, it can disrupt the normal flow of enzymes, leading to irritation and, in rare cases, pancreatitis.
The reassuring news is that while pancreatitis is listed as a possible side effect, it’s actually quite rare. Studies show it affects only about 0.5% of every 1,000 people taking GLP-1 medications like Ozempic® and Wegovy®. What does this mean for you? While it’s something to be aware of, if you don’t have risk factors, it’s likely not something you will experience.
Pancreatitis: Symptoms, risks, and warnings
While most people won’t experience pancreatitis from taking Ozempic®, Wegovy®, or another GLP-1 medication, recognizing the signs early is key. Why? Pancreatitis is a medical emergency. If you notice symptoms, you need to go to the nearest emergency room right away to get treatment.
Here are the most common symptoms of pancreatitis:
- Severe upper abdominal pain that may radiate to your back and doesn’t ease with position changes or pain relievers
- Ongoing nausea and vomiting that won’t go away
- A fever, often accompanied by chills
- A rapid heartbeat that feels out of the ordinary
When can you get pancreatitis from a GLP-1 medication
In the rare case that someone develops pancreatitis, symptoms usually appear within the first few weeks or months after starting Ozempic® or Wegovy®. Though they can develop at any point during treatment, even after you’ve been on the medication for a while.
Because symptoms can show up at any time, it’s important to stay tuned into how your body feels throughout treatment.
If you ever notice symptoms of pancreatitis, stop taking the medication and seek emergency care right away. Getting treated quickly can reduce the risk of serious complications and help you and your provider decide the safest path forward.
Rx weight loss, the right way, with Noom
Get access to prescription weight loss medication with Noom.What the research says about Ozempic® and Wegovy® and pancreatitis risk
When it comes to the risk of pancreatitis with Ozempic® and Wegovy®, multiple large studies suggest that these medications, while not risk-free, don’t significantly increase the chance of developing pancreatitis for most people. Here’s some research:
- A comprehensive study involving over 34,000 people taking semaglutide found no significant rise in pancreatitis risk compared to those using other treatments.
- Another study involving over 4 million people found that those taking semaglutide and liraglutide had a slightly higher relative risk of pancreatitis compared to those using bupropion-naltrexone (Contrave) or orlistat (Alli and Xenical). Despite the slight increase, the overall risk remained very low at around 0.5% in every 1,000 people.
- The FDA’s own development data for semaglutide showed no increased risk of pancreatitis among people compared to those taking a placebo. This included both people with type 2 diabetes and those using the medication for weight management.
- Even with safety monitoring systems like the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) logging hundreds of reported cases over time, no direct causal relationship has been confirmed.
What this all means is that pancreatitis is a rare side effect, in the context of how widely these medications are used. Millions of people have taken Ozempic®, Wegovy®, and similar GLP-1 medications safely.
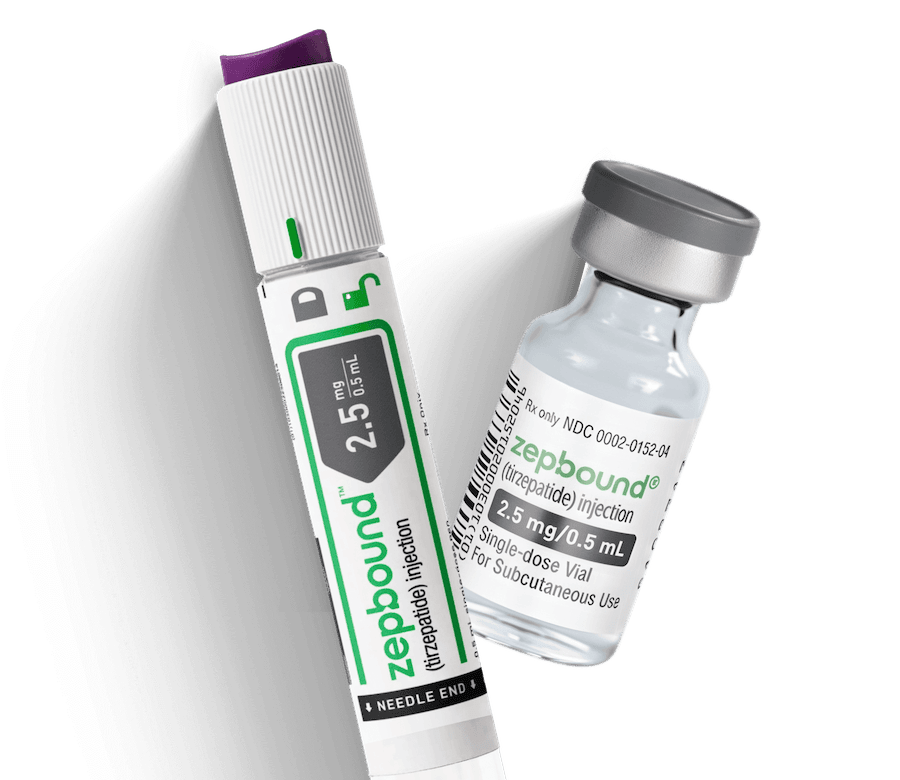
What about tirzepatide medications? Are Mounjaro® or Zepbound® linked with pancreatitis?
Tirzepatide works a bit differently from medications made with semaglutide, like Ozempic® and Wegovy®. It activates another set of receptors (GIP) along with GLP-1. When it comes to the risk of pancreatitis, the data so far suggest that tirzepatide doesn’t significantly increase that risk overall.
A recent review involving nearly 10,000 people found no clear increase in pancreatitis risk—the results suggested a possible higher risk, but they were too uncertain to say for sure. Another review showed that while some people experienced elevated pancreatic enzyme levels, this did not translate into more cases of pancreatitis, and again, the data were inconclusive. A few case reports do show that pancreatitis can happen suddenly and be life-threatening.
Still, pancreatitis remains very rare compared to the millions who’ve taken these medications safely. If you develop severe abdominal pain, persistent nausea, vomiting, or fever while on Mounjaro® or Zepbound®, stop the medication and get medical help right away.
Ozempic®/Wegovy® and pancreatitis: Who should use extra caution or avoid GLP-1s?
Most people can take GLP-1 medications like Ozempic® and Wegovy® safely under medical supervision. But when it comes to pancreatitis, certain health factors can raise your risk. If any of these apply to you, make sure to discuss them with your doctor when considering GLP-1s.
- People with a history of pancreatitis are at higher risk of developing it again.
- People with gallbladder disease or gallstones need careful monitoring. Research shows that GLP-1 medications can increase the relative risk of gallbladder problems, which can lead to pancreatitis in rare cases.
- People with very high triglyceride levels should work closely with their healthcare provider to manage these levels before starting treatment, as elevated triglycerides are a known pancreatitis risk factor.
- People who drink heavily (over eight drinks for women and over 15 for men per week) should address their alcohol consumption before beginning GLP-1 therapy. Alcohol is a major cause of pancreatitis, and combining it with these medications increases the risk.
Can I restart GLP-1 medication if I experience symptoms of pancreatitis?
Anyone who develops pancreatitis symptoms while taking these medications must stop treatment immediately. They can only consider restarting after a thorough evaluation and discussion with their healthcare provider about whether the benefits outweigh the risks. In the case of tirzepatide (Mounjaro®/Zepbound®), the prescribing information specifically warns that treatment should only be restarted if the benefits clearly outweigh the risks and your provider agrees it’s safe to do so.
Are there any ways to reduce pancreatitis risk
You can’t completely remove every risk factor for pancreatitis, but you can take practical steps to support your pancreas and lower your chances of problems while using Ozempic® or GLP-1 medications.
- Follow a balanced, lower-fat eating pattern: Build your meals around fruits, vegetables, lean proteins, and whole grains with some healthy fat. Limit total daily fat intake to about 20 to 35% of your calories (roughly 30 to 50 grams for most adults) to reduce strain on your pancreas. Avoid fried and heavily processed foods, which can increase the risk of gallstones, a leading cause of pancreatitis.
- Pace your weight loss: Aim for slow, steady progress of around 1 to 2 pounds per week. Losing weight too quickly can lead to gallstone formation, which may trigger pancreatitis. If you’re just starting your GLP-1 medication, closely follow your titration schedule to help reduce side effects and support safer, more sustainable weight loss. In some cases, people can stay on lower doses if needed.
- Stay hydrated and eat smaller meals: Drinking enough water and eating smaller, more frequent meals can help ease digestion and reduce the workload on your pancreas, especially as your body adjusts to GLP-1 medications.
- Watch for warning signs: Seek immediate medical care if you experience severe upper abdominal pain, persistent nausea, vomiting, or fever. These could be signs of pancreatitis, and delaying care can make complications more likely.
- Schedule regular check-ins with your healthcare provider: Ongoing medical supervision allows your provider to monitor your progress, adjust your treatment plan, and address any early warning signs.
- Limit alcohol: Drinking heavily is a leading cause of pancreatitis, and combining alcohol with GLP-1 medications may increase your risk. Cutting back or eliminating alcohol can help protect your pancreas.
- Avoid smoking: Smoking is also linked to a higher risk of pancreatitis. Quitting not only benefits your pancreas but also supports your overall health and long-term wellness.
By combining these preventive steps with open communication with your healthcare team, you can use GLP-1 medications more safely while still working toward your long-term health goals.
Frequently asked questions about Ozempic®/Wegovy® and pancreatitis
Here are some of the most common concerns about pancreatitis that people bring up with their healthcare providers when considering GLP-1 treatment.
What are the pancreatitis symptoms I should look for while taking Ozempic®, Wegovy®, or another GLP-1 medication?
The most important warning signs include severe upper abdominal pain that often spreads to your back, persistent nausea and vomiting that won’t stop, and fever with a rapid heartbeat. These symptoms are different from the common digestive side effects many people experience when starting Ozempic®. Pancreatitis pain is typically much more intense and doesn’t improve with position changes or over-the-counter remedies.
How soon can pancreatitis happen after starting Ozempic® or Wegovy®?
Pancreatitis can develop at any time during treatment, but most cases occur within weeks to months of starting the medication.
Is the pancreatitis risk the same for other semaglutide (Rybelsus®) and tirzepaide (Zepbound® and Mounjaro®) medications?
All GLP-1 medications carry similar pancreatitis warnings, though the exact risk may vary slightly between different medications in this class. Rybelsus® contains semaglutide like Ozempic® and Wegovy®, so it shares the same risk profile, while Mounjaro® and Zepbound® contain tirzepatide and work on additional hormone receptors. The medical guidance remains consistent across all these medications: If pancreatitis symptoms develop, discontinue treatment right away and get emergency medical help.
Are people with a history of pancreatitis at higher risk?
Yes, people with a previous history of pancreatitis face a higher risk when using GLP-1 medications. Other factors that increase risk include gallbladder disease, very high triglyceride levels, and heavy alcohol use. Your healthcare provider can help you weigh these risk factors against the potential benefits to determine if these medications align with your health goals.
The bottom line: The risk of pancreatitis with Ozempic®, Wegovy®, and other GLP-1 medications
When you step back and look at all the research, the message is somewhat reassuring: pancreatitis is rare and, for most people, the overall risk is low. Millions have used these treatments safely. The key is knowing the warning signs so you can act quickly if they appear. Understanding your personal risk factors, such as a history of pancreatitis or gallbladder issues, allows you and your healthcare provider to make the most informed decision for your situation.
Taking charge of your health is about more than just starting a medication; it’s about having the right support every step of the way. If you qualify for Noom Med, you’ll be paired with a clinician who can find the right medication for you and prescribe it if needed. Then they’ll be with you from your smartphone to help monitor side effects, track symptoms, and build and maintain healthy habits to help you work toward your goals.
Note: Ozempic®, Rybelsus®, and Mounjaro® are not FDA-approved to treat obesity or for weight loss.
Why you can trust us
At Noom, we’re committed to providing health information that’s grounded in reliable science and expert review. Our content is created with the support of qualified professionals and based on well-established research from trusted medical and scientific organizations. Learn more about the experts behind our content on our Health Expert Team page.



















 Noom Team
Noom Team
 Shoshana Fishbein
Shoshana Fishbein


 Meaghan Cameron
Meaghan Cameron